Brief Recap
This series of articles is about using personal data to manage or improve health. After considering why it might be a good idea for people to keep a complete set of their own medical records (including vaccine records), I began to dig deeper into one specific type of data many people care about: nutrition and metabolism.
Part I looked at three eras in the past 125 years of American nutrition data.
(~1890s – 1945) Nutrition science measured food as fuel for physical work.
(~1950 – 2005) Food became a consumer product for organized businesses.
(~2007 – present) Digital media became a battleground for food ideologies. Your clicks are valuable.
Part II looked at nutritional data as a test case for a new kind of personal health record, and asked whether personal ownership of health data might provide some benefits. It would be interesting if we could simply calculate our nutritional needs by measuring our own physical work, but there are many reasons that this is not practical. Precise measurement of calories in and calories out is very difficult. Nonetheless a simple notebook approach to self-assessment of your current diet can provide very useful insights. For example:
What is the macronutrient ratio (relative carbohydrate/protein/fat calories) in your diet?
How much fiber do you eat? How much salt? How much sugar?
If you want to perform simple self-experiments involving nutrition, logging your data allows you to develop insights into what works for you. For example:
When you change your diet, what happens to your biomarkers (such as blood tests for cholesterol, triglycerides, and hemoglobin A1c?)
If you decide to increase fiber intake, what changes result?
Here in Part III, the idea is to look at how biomarkers might be useful for assessing your nutritional and metabolic health.
You and Your Biomarkers
The conventional approach to seeing your medical test results often begins and ends with “Ask your doctor.” Or, “See a nutrition professional before making any changes.” Yet many folks ask their doctor about what to eat – and are frustrated by brief and not particularly helpful nutritional guidance. And so while I am steeped in the traditions of Western medicine, I think that “ask your doctor” is kind of a stupid place to start talking about diet and metabolic tests. Asking your grandmother is easier. Asking yourself, by Thinking About Your Own Health can also be a great start, especially if you can learn to do it with a bit of scientific objectivity. Even if you do need specialized help with nutritional management of your metabolic disease, gastrointestinal disease, kidney disease, or anything else, an intellectually honest and caring healthcare professional would usually admit that it’s easier to help a patient who has already gathered some basic information by paying attention to their own body. In most US states, you can even order your own blood tests without ever having to go see a doctor – it’s called Direct Access Testing. What about recording some metabolic biomarkers in your notebook?
Let’s say Mr. Duffer has access to a web portal that allows him to see the lab tests his doctor ordered at the last checkup. This is sometimes called a “tethered Personal Health Record.” It’s data about him, but he doesn’t control it because it’s tethered to a hospital or clinic’s Electronic Medical Record, EMR.
The lab report says that normal glucose (blood sugar) is 65 – 99 mg/dL. The normal range assumes that Mr. Duffer was “fasting” when he had his blood drawn. But what the laboratory (and the tethered PHR) don’t know is that Mr. Duffer ate a big bowl of Cap’n Crunch just half an hour before he went to the lab. His result: glucose = 180. The lab flags this result with a big red highlighter -- not normal! His blood sugar is high.
Can we give Mr. Duffer a diagnosis? No. Does he have a disease? Maybe not. It’s normal for a healthy person’s blood glucose to rise after eating. The speed and extent of that rise depends on the person’s metabolic health, but also on the food. You might have heard about the “glycemic index” of foods – a high glycemic index suggests that a food causes the blood sugar to rise more. The word “spike” is tossed around to make this sound scary. But the blood sugar rise also depends on what else was eaten, and in what order, the time of day, the speed of the stomach emptying into the small intestine, and lots of other factors.
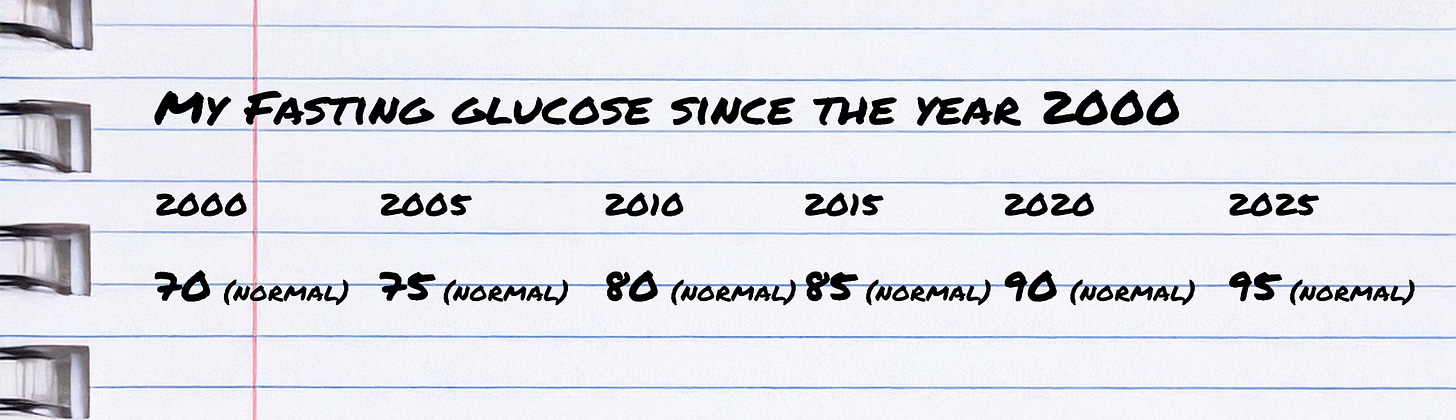
Unlike her husband, Mrs. Duffer takes great care always to be “fasting” when she gets her blood drawn. Look at her notebook:
Figure 1: Mrs. Duffer is an organized person who has kept all her results in a table for many years. And every year, her glucose was in the normal range (66-99), so that’s great, right? Or is there something more to be learned?
All her glucose results are normal too — within the normal range. But I’ll bet you see it already — over 25 years, Mrs. Duffer’s fasting glucose has steadily increased. (Very steadily – since both she and her numbers are fictional and simplified.) Patterns in one person’s lab test results over time can provide useful information, even if they are all within the normal range. Maybe it’s the kind of information you are looking for if you’re reading this.
Does Mrs. Duffer have something going on that she ought to know about? There are always alternative explanations, to be sure – maybe what looks like a trend is actually just a random pattern, or was caused by something else. But the trend of glucose rising over the years (even within the range defined as “normal”) might indicate that something about Mrs. Duffer’s metabolism is changing.
Recording more data in her notebook (weight, waist circumference, or other blood tests, for example) could have increased its power to suggest what’s going on. Of course, too much data risks losing sight of what’s important. But a good doctor who saw the 25 year trend of her glucose would probably suggest getting more information. Even though she’s got a good doctor now, Mrs. Duffer has moved around the country and had three different doctors over the past 25 years. As a result, she is actually the only person who is really in a position to see the long-term trend of this biomarker rising.
What are biomarkers anyway?
A biomarker is something you can measure which is an indicator of a biological condition. Usually a biomarker refers to a molecule in the blood that can be measured, like glucose in Mr. and Mrs. Duffers’ examples above. Many biomarker numbers are “continuous measurements” – that is, they are not a “test is positive” or “test is negative” kind of result, but rather they are a number on a quantitative scale. Even though all of Mrs. Duffer’s measurements are in the normal range, and she may not yet quality for a diagnosis of diabetes or even pre-diabetes, nonetheless a common explanation for her results is that over the years she is becoming less sensitive to insulin.
While you’ve heard a lot lately about the price of insulin (the pharmaceutical product for treating diabetes) remember that your body — your pancreas, really — produces insulin. Normally insulin is released from your pancreas after eating, and it activates cells to take up glucose from the blood.
Insulin resistance is at the center of many conditions including diabetes, cardiovascular diseases, kidney diseases, erectile dysfunction, and dementia. These can be considered together as metabolic diseases. Trust me -- you’d like to avoid becoming insulin resistant. And it is a really big problem. Nearly half of young adult Americans have insulin resistance! They are on a path to cardiovascular disease and other complications. And though I think that much of “longevity” medicine is nonsense, preventing or combating insulin resistance will almost certainly improve your odds of staying alive.
Besides simple tests like blood glucose, other much more complex signals could also be biomarkers; for example, some people are very interested in how the human intestinal microbiome might affect health. Is a gut microbiome test a biomarker? Instead of a single number every time you measure your glucose level, even a one-time assessment of the microbiome would produce a large set of data. If you went to the trouble of finding out the hundreds of species of bacteria in your poop and their relative proportions, it might be interesting but it’s not so easy to show how that might be associated with or cause health outcomes, and so in most circumstances there’s not a good reason today to go looking for a microbiome test. Maybe next year I’ll think differently. Right now I would not call this a biomarker. If you’ve got spare time and resources to investigate your body, I’d suggest starting with things that can clearly make a difference — like metabolic health.
Certain physical measurements like blood pressure have also come to be considered as biomarkers. Today our digital and wearable devices have the potential to provide data that could become biomarkers. Heart Rate Variability (HRV), for example, refers to the measurement of subtle beat-to-beat differences in heart rate. HRV can be used as a biomarker, since the heart’s internal pacemaker varies with changes in our nervous system, hormones, and other influences. Can you add HRV data to your notebook? Yes, but it might not be easy. Who owns your HRV data? Gadgets that capture and process your data want to sell it back to you as a marker of health, of recovery from exercise, and as part of a fitness coaching algorithm. Are you confident in the method that your gadget uses to measure it? Some skepticism is warranted unless you are very careful about getting a perfect signal. And raw data ownership might be a concern when your gadget’s subscription runs out. A great source of information if you want to study up on HRV is at Marco Altini’s Substack.
For Thinking About Your Own Health, the most useful biomarkers are not only early indicators of risk, but are also barometers of how well a prevention or treatment strategy is working. Biomarkers that look at metabolic health are likely to meet this standard. Using any biomarker requires attention to methodology, sources of error, and applicability for health. So, if the intention was to use fasting morning blood sugar as a screening test for insulin resistance, then Mr. Duffer’s high glycemic breakfast cereal created a flaw in his data-gathering method. To be your own scientist, or your own maintenance engineer, you’ll have to be careful.
Metabolic Health and Insulin Sensitivity: Biomarkers in Action
So how could a thinking person use biomarkers to understand their metabolism? Besides glucose, a couple of other useful biomarkers are the blood tests insulin and hemoglobin A1c.
In most adults with insulin resistance, the pancreas responds by making more insulin, and so insulin levels rise. But those tests represent a single point in time, so they are highly susceptible to what was happening just then. You didn’t eat Cap’n Crunch, but even if you just had coffee with creamer in the morning before you went to get your blood drawn, the glucose and insulin result could be influenced quite a lot. The hemoglobin A1c test, on the other hand, is an indicator of the average blood sugar level over the prior 90-120 days, and so it can be another useful biomarker if you want to keep an eye out for developing insulin resistance.
Figure 2: Insulin Resistance affects cells everywhere, but muscle, liver, and fat cells are especially important.
Science nerd section: How insulin resistance works
The typical cascade of metabolic disease begins with chronic over-nourishment, where calorie intake consistently exceeds calorie expenditure. In genetically susceptible people, over time this leads to increased fat storage. Expanding adipose (fat) tissue releases higher levels of inflammatory signaling molecules, contributing to systemic inflammation and further impairing metabolic function.
Normally, insulin causes cells to take up glucose from the blood. In response to excess energy and inflammation, cells in skeletal muscle, liver, and fat become less responsive to insulin. This is called insulin resistance. To compensate, the pancreas may produce more insulin, resulting in elevated insulin levels in blood.
As insulin resistance progresses, adipose tissue's capacity to store fat is overwhelmed, and fatty acids spill into the bloodstream. These fatty acids may be deposited in non-adipose tissues, including liver and skeletal muscle, where they accumulate and disrupt normal metabolism. The combination of free fatty acids, excess insulin, uncontrolled glucose, and inflammation is particularly bad for the lining of arteries. Many of the worst complications of insulin resistance (such as heart disease, stroke, etc) result from its effects on diseased arteries.
Skeletal muscle tissue (the various muscles that move your body) normally accounts for the majority of insulin-stimulated glucose uptake. Fat accumulation and inflammation reduce muscle’s ability to take up and utilize glucose. While insulin resistance develops in many other tissues, skeletal muscle is both the largest site for glucose disposal and also the earliest site of resistance. These changes can occur many years before diabetes or metabolic diseases are diagnosed, suggesting that early detection may provide important opportunities for prevention.
If fasting glucose, insulin, and hemoglobin A1c tests allow me to keep an eye out for insulin resistance, what good does monitoring myself do?
In these essays I try pretty hard to distinguish between ideas that are well-supported by evidence, and ideas that are just ideas. So the answer to this question is an idea, and this could be its hypothesis:
Compare a person who monitored their own biomarkers, versus a person who did not. Imagine that the biomarker dashboard shows something interesting. By noticing these patterns early, (we could hypothesize that) compared to the control (an identical person who didn’t keep a notebook) the notebook user would learn whether the diet/exercise/lifestyle strategies they try actually work to move their biomarkers in a specific targeted direction and would be more likely to achieve goals of metabolic health. (Now, that still doesn’t prove that it would make them live longer, right? But it might be a pretty good indicator.)
What could you do to try to improve your metabolic biomarkers?
For many people a cause of insulin resistance is over-nourishment, a chronic imbalance between the total calories taken in and the total energy expended (calories out). However it is also quite possible for some genetically predisposed people to have insulin resistance without being overweight. Genetics plays a big role in your susceptibility to get insulin resistant. You can’t pick new parents.
Correcting over-nourishment is notoriously hard. Energy balance can be affected by doing more physical activity, but bear in mind that 45 minutes of moderately difficult exercise on the stationary bike only burns 200 – 500 calories, or between four and ten Oreo cookies.
Eat less, burn more
As an approach to combating over-nourishment, the advice to “eat less and exercise more” is both fundamentally correct, and also generally not helpful as advice for people who struggle to lose weight. Besides changing the balance of your personal total CI/CO (calories in / calories out) equation to avoid or reverse over-nourishment, there are other things you can try which might change your sensitivity to insulin.
Change foods
The ratio of dietary macronutrients (carbohydrates, proteins, fats), the timing of eating, sugar consumption, and fiber in the diet all can affect the trend towards insulin resistance and metabolic disease. There might be something especially good about the Mediterranean Diet. (In this diet, carbohydrates are ~40% of total calories, emphasizing whole grains, fruits, and vegetables; protein is ~15-20% of total calories and includes lean meats, fish, and plant-based proteins; fats are around 35-40%, particularly unsaturated fats from sources like olive oil, nuts, and avocados.)
Change schedules too; but try extreme diets only with caution
There’s pretty good evidence to suggest that time-restricted eating (for example, eating only during the first part of the day and not eating in the evening) or periods of fasting may make some insulin-resistant people recover their responsiveness to their body’s own insulin. Proponents of the popular ketogenic diet suggest that it may have a similar effect. Cautious clinicians may sometimes consider these as short-term strategies but not a lifelong approach, and I’m concerned that the ketogenic diet in particular (very very low carbohydrate, high fat and protein) may accelerate the development of heart disease in some people.
Get strong
To make more insulin-responsive tissue, you can build muscle. One of the reasons that more people become insulin resistant with aging is that they have lost skeletal muscle, and this is one of dozens of arguments that I’ll make for the health benefits of resistance exercise. Because muscle is the largest contributor to insulin-triggered glucose uptake, adding muscle through purposeful strength training can be an extremely effective way to combat insulin resistance.
Get fit
Increasing endurance, both with high-intensity interval training and with moderate-intensity longer duration exercise can improve cells’ ability to burn fat as an energy source. When fat can be used as fuel, it reduces the tendency for fatty acids to accumulate in the liver and muscle, interrupting the cascade of insulin resistance.
Get sleep
A surprising number of people can improve their metabolic health by getting more/better quality sleep, including treating sleep-disordered breathing or sleep apnea if present.
Pitfalls: When Biomarkers Might Lead Us Astray
You’ve probably seen a device that provides a constant stream of biomarker data to explore. The Continuous Glucose Monitor (CGM) was developed for people with diabetes who need to inject insulin, but today plenty of people are wearing a little CGM patch on their upper arm to explore their own metabolism. It takes glucose measurements every few minutes. Medical professionals are divided: some wish that these would be restricted to use by people with diabetes under medical oversight. They worry that when people see their glucose levels rise after eating healthy foods, they’ll be tempted to restrict their carbohydrate intake more than they should. “They’ll get scared by a perfectly normal glucose spike and decide they should avoid blueberries and eat only bacon!” goes the argument.
An opposing argument has its basis in principles of data ownership. “It’s my body, and this device is quite safe for me to use to see what’s going on with my blood sugar.” You can monitor your car’s fuel consumption — you own it, and you decide whether to maintain it. Perhaps it should be the same way with your body – that it should be up to you to decide what you do with the data. I’m hypothesizing that it’s possible for people to learn how to interpret their own biomarkers like CGM data, fasting glucose, insulin, and hemoglobin A1c. Maybe their data could inform good health choices. Maybe it could allow early recognition of metabolic disease (years before the development of type 2 diabetes that sends them to the doctor or the emergency room.) Maybe it could provide a more sensitive tool for deciding when it’s time to take a few weeks off from eating ice cream before bed.
Figure 3: Some truly committed self-experimenters have used the CGM (Continuous Glucose Monitor) together with defined protocols like the Oral Glucose Tolerance Test, ingesting 75 grams of glucose syrup and watching the resulting peak in blood glucose, followed by the insulin-driven response as glucose is drawn into cells, causing the blood glucose level to fall.
To be clear: the all-bacon diet is almost certainly a bad idea. But I am intrigued by the possibility that some folks who are committed to careful self-curated health will be able to learn useful things by watching their nearly real-time results from a CGM. We could certainly imagine that when Mr. Duffer sees the connection between that big bowl of Cap’n Crunch and the dramatic rise and fall of his blood sugar, it could be an effective learning strategy for him to improve his diet. Maybe better than being scolded by his doctor on the way out the door to “eat a Mediterranean diet and watch your weight.” I would bet that a combination of self-curated data plus professional guidance might be the best approach.
That said, if you uncover something that’s maybe a bit concerning about your health, I hope that you’ve got access to a doctor (or a nurse practitioner) who can look at the information and help you figure it out. Maybe what you really need is another kind of test. Maybe the safest or best approach will be to start you on a prescription medicine right now, to get your metabolism under control, even if your hope is eventually to change your diet and lifestyle so that medicine is no longer needed.
I don’t think you need to believe in extreme libertarian tech ideals, or to be skeptical about healthcare, or to be an edge case biohacker to want to know how your body is handling the foods you eat as fuel for the life you’re living. Most people keep track of their weight and whether their jeans fit. They can do this on their own, and don’t need to ask their doctors what the results mean. If you’ve got a wonderful attentive doctor working with you on metabolic health, then that’s fantastic! But most people don’t have that luxury, and the health care industry is not doing a great job in general of preventing metabolic disease. To be clear, self-directed blood testing is a bit controversial, and not so much the “standard of care” with scientific evidence. But I’m suggesting here that when Thinking About Your Own Health, a scientific approach to monitoring some simple biomarkers might improve your ability to keep track of how you’re doing, and maybe even to figure out how to do better.
What do you think?
Unfortunately there is a lot of bullsh*t health advice out there too, so a smart person Thinking About Their Own Health might want some guardrails to help them avoid crazy diets. They might want trustworthy advice about interpreting the data and when to ask for professional help. Where can you get that advice?
What do you think? Would you ever feel comfortable ordering basic blood tests for yourself? Buying a continuous glucose monitor and interpreting the results on your own? What other biomarkers would you like to learn about?






Hi there,
I enjoyed your writing. I’ve spent the past 30 years as a gastroenterologist in Cleveland, and I've also spent 16 of those years writing about my work. I just created a Substack in the hopes of generating dialogue about issues in the medical world. My latest post is about when patients (especially aging patients) reject colonoscopies—and the questions that raises about healthcare autonomy. I'd be really interested to hear your thoughts, and I hope you might consider following my work. Be well!
https://mkirsch.substack.com/p/when-should-a-patient-reject-colonoscopy